
Tips for Effective SOAP Notes
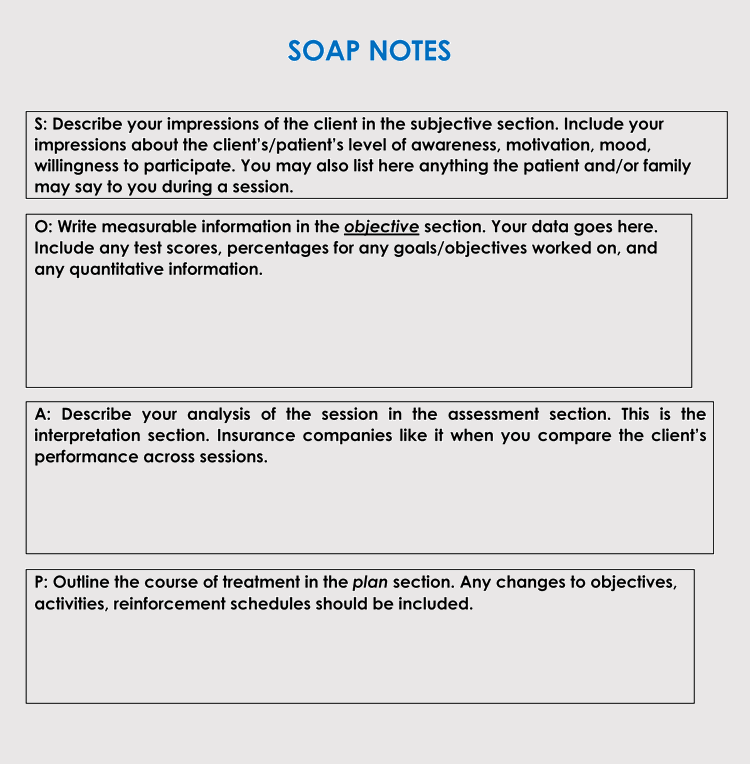
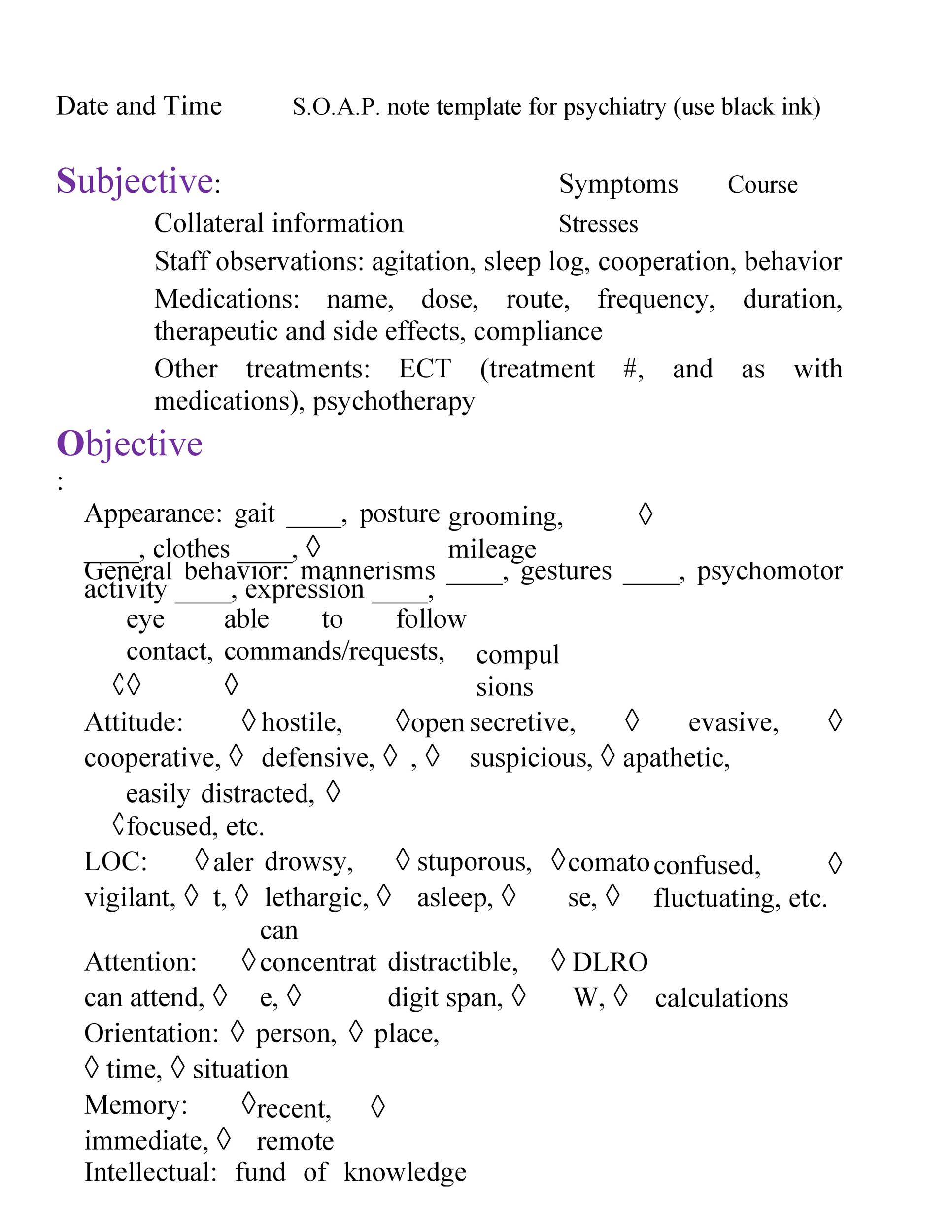
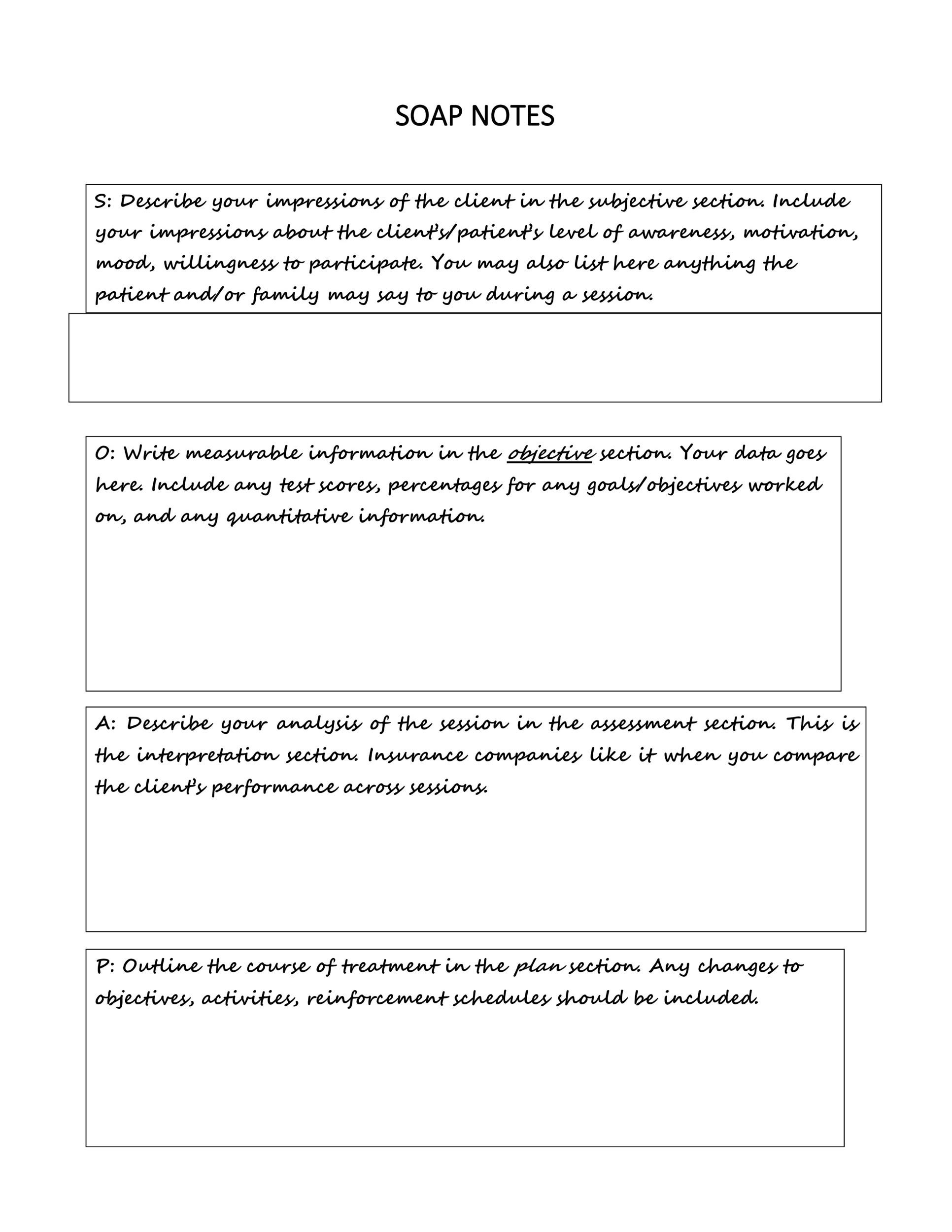
· We understand that writing SOAP Notes can be challenging, especially if it is your first. Therefore, based on the knowledge of our best nursing writers, we have compiled a step-by-step guide to help you write one comfortably. We begin by defining the SOAP Notes to understand what's behind the acronym Writing effective SOAP notes is a critical aspect of effective and accurate documentation for chiropractors. SOAP notes need to be concise, clear, and thorough. They should include the patient’s injury, when the injury began, results of tests and assessments, treatments and any progress that has been observed · A SOAP (subjective, objective, assessment, plan) note is a method of documentation used specifically by healthcare providers. SOAP notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way. SOAP notes, once written, are most commonly found in a patient’s chart or electronic medical blogger.comted Reading Time: 8 mins
Download Our Editable SOAP Note Templates
SOAP notes are only a tool to help practitioners. We are going to highlight tips for effective SOAP notes. Write SOAP notes at the appropriate times. Avoid writing SOAP notes when you’re seeing your patient. You should be taking personal notes to help you write your SOAP notes later. Also, try not to wait too long to create your SOAP notes · An important part of patient Electronic Health Records, SOAP notes should be legible and make use of professional jargon to serve as a common frame of reference. They should be written in the present tense. Concise and specific Tips for completing SOAP notes: Consider how the patient is represented: avoid using words like “good” or “bad” or any other words that suggest moral Avoid using tentative language such as “may” or “seems” Avoid using absolutes such as “always” and “never” Write legibly Use language common to the
What are SOAP Notes?
Writing effective SOAP notes is a critical aspect of effective and accurate documentation for chiropractors. SOAP notes need to be concise, clear, and thorough. They should include the patient’s injury, when the injury began, results of tests and assessments, treatments and any progress that has been observed · An important part of patient Electronic Health Records, SOAP notes should be legible and make use of professional jargon to serve as a common frame of reference. They should be written in the present tense. Concise and specific Tips for Effective SOAP Notes. Find the appropriate time to write SOAP notes. Avoid: Writing SOAP Notes while you are in the session with a patient or client. You should take personal notes for yourself that you can use to help you write SOAP notes. Avoid: Waiting too long after your session with a client or a patient has ended

What’s the SOAP note definition?
SOAP notes are only a tool to help practitioners. We are going to highlight tips for effective SOAP notes. Write SOAP notes at the appropriate times. Avoid writing SOAP notes when you’re seeing your patient. You should be taking personal notes to help you write your SOAP notes later. Also, try not to wait too long to create your SOAP notes · We understand that writing SOAP Notes can be challenging, especially if it is your first. Therefore, based on the knowledge of our best nursing writers, we have compiled a step-by-step guide to help you write one comfortably. We begin by defining the SOAP Notes to understand what's behind the acronym · An important part of patient Electronic Health Records, SOAP notes should be legible and make use of professional jargon to serve as a common frame of reference. They should be written in the present tense. Concise and specific
3 Helpful Templates and Formats
· A SOAP (subjective, objective, assessment, plan) note is a method of documentation used specifically by healthcare providers. SOAP notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way. SOAP notes, once written, are most commonly found in a patient’s chart or electronic medical blogger.comted Reading Time: 8 mins Writing effective SOAP notes is a critical aspect of effective and accurate documentation for chiropractors. SOAP notes need to be concise, clear, and thorough. They should include the patient’s injury, when the injury began, results of tests and assessments, treatments and any progress that has been observed · An important part of patient Electronic Health Records, SOAP notes should be legible and make use of professional jargon to serve as a common frame of reference. They should be written in the present tense. Concise and specific
No comments:
Post a Comment